-
-
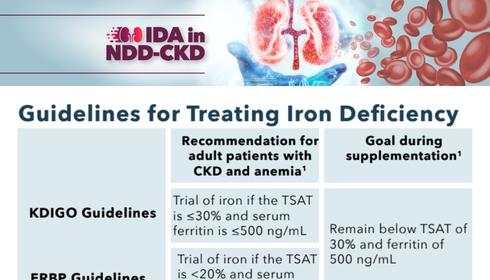
CME/CE activities that overview in detail the screening, diagnosis, and treatment of IDA in NDD-CKD
CME/CE Activities
-
-
Helpful patient education materials and frequently-asked questions about IDA in NDD-CKD
Patient Resources
-
Short videos offering expert clinical pearls on the diagnosis and treatment of IDA in NDD-CKD
Expert Commentary
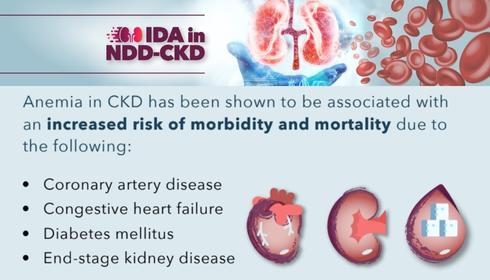
Iron deficiency anemia (IDA) is a common condition in patients with non–dialysis-dependent chronic kidney disease (NDD-CKD) that can affect quality of life and exacerbate morbidity. Despite the impacts of IDA in NDD-CKD patients, its screening, diagnosis, and treatment remains challenging. This educational hub will aim to increase awareness about IDA in this setting, as well as provide informational resources to clinicians about risk factors, diagnosis, and treatment of IDA in NDD-CKD patients.
Are you a provider or patient that wants to stay connected about IDA in NDD-CKD?
Click the button below to stay connected:
CME/CE Activities
Expert Commentary

Orlando Gutierrez, MD, MMSc
Dr. Gutiérrez serves as the Marie S. Ingalls Endowed Chair in Nephrology Leadership and is professor of medicine and director of the Division of Nephrology at the University of Alabama at Birmingham. His work as a physician-scientist focuses on mineral metabolism in patients with kidney failure and chronic kidney disease. Dr. Gutiérrez earned his medical degree from the University of Toledo College of Medicine and trained in internal medicine, nephrology, and clinical research at the Massachusetts General Hospital. He received a Master of Medical Science degree from Harvard Medical School.

Kamyar Kalantar-Zadeh, MD, MPH, PhD
Dr. Kalantar-Zadeh is professor of medicine, pediatrics, public health and nursing sciences at the University of California. In his clinical research, Dr. Kalantar-Zadeh studies outcomes and epidemiology of kidney disease with a focus on anemia and iron deficiency. He studied medicine at the Universities of Bonn and Nuremberg in Germany and earned a Master of Public Health and PhD in epidemiology from the University of California Berkeley. Dr. Kalantar-Zadeh’s postgraduate training included a pediatric medicine residency at the State University of New York Brooklyn and a nephrology fellowship at the University of California San Francisco.
Videos:
Impacts & Screening of IDA in NDD-CKD
Treatment of IDA in NDD-CKD: Perspectives & Considerations
Clinician Resources
Patient Resources
IDA IN NDD-CKD WHAT YOU SHOULD KNOW
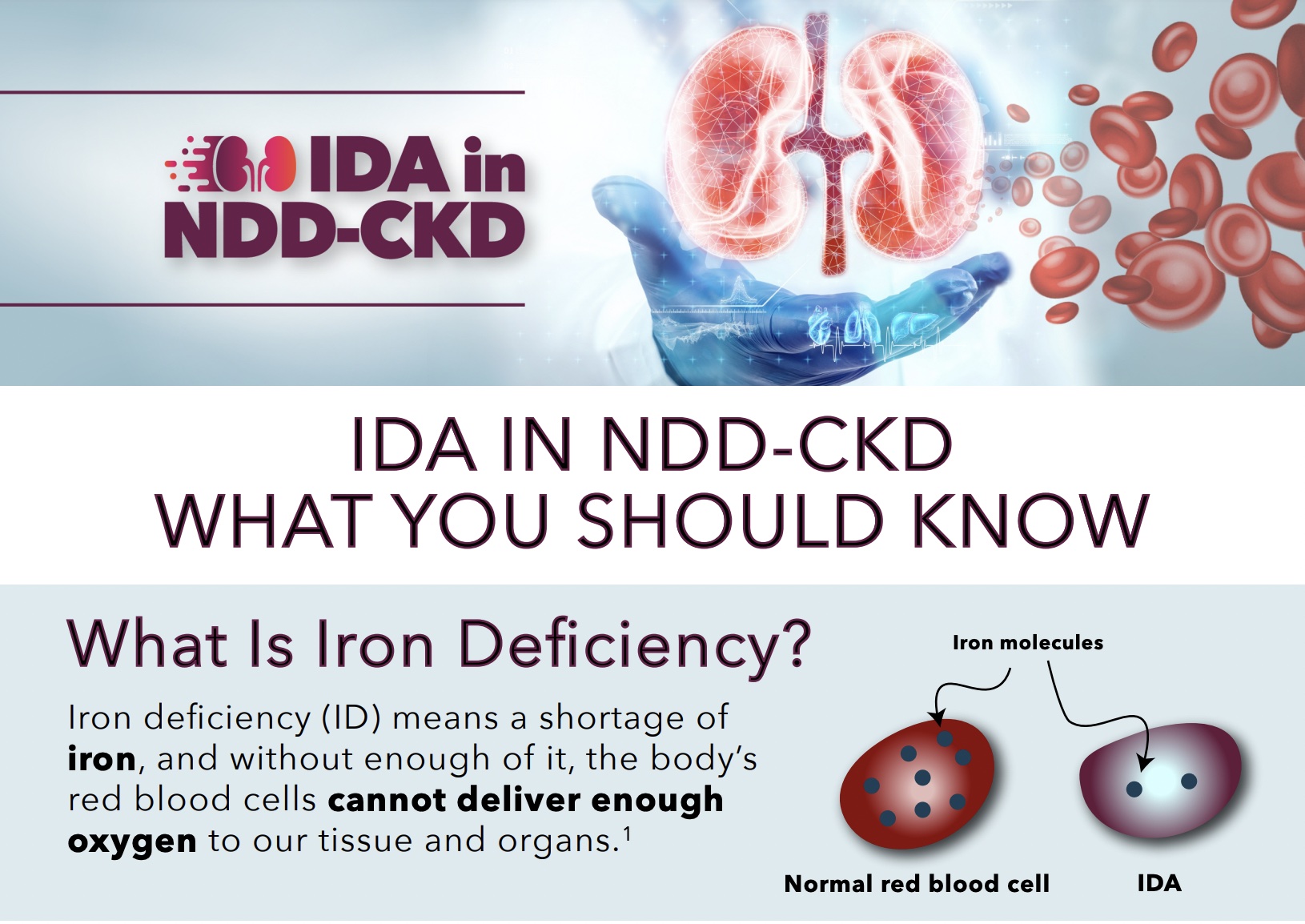
What Is Iron Deficiency? Iron deficiency (ID) means a shortage of iron, and without enough of it, the
HOW IS IDA IN NDD-CKD DIAGNOSED AND TREATED?
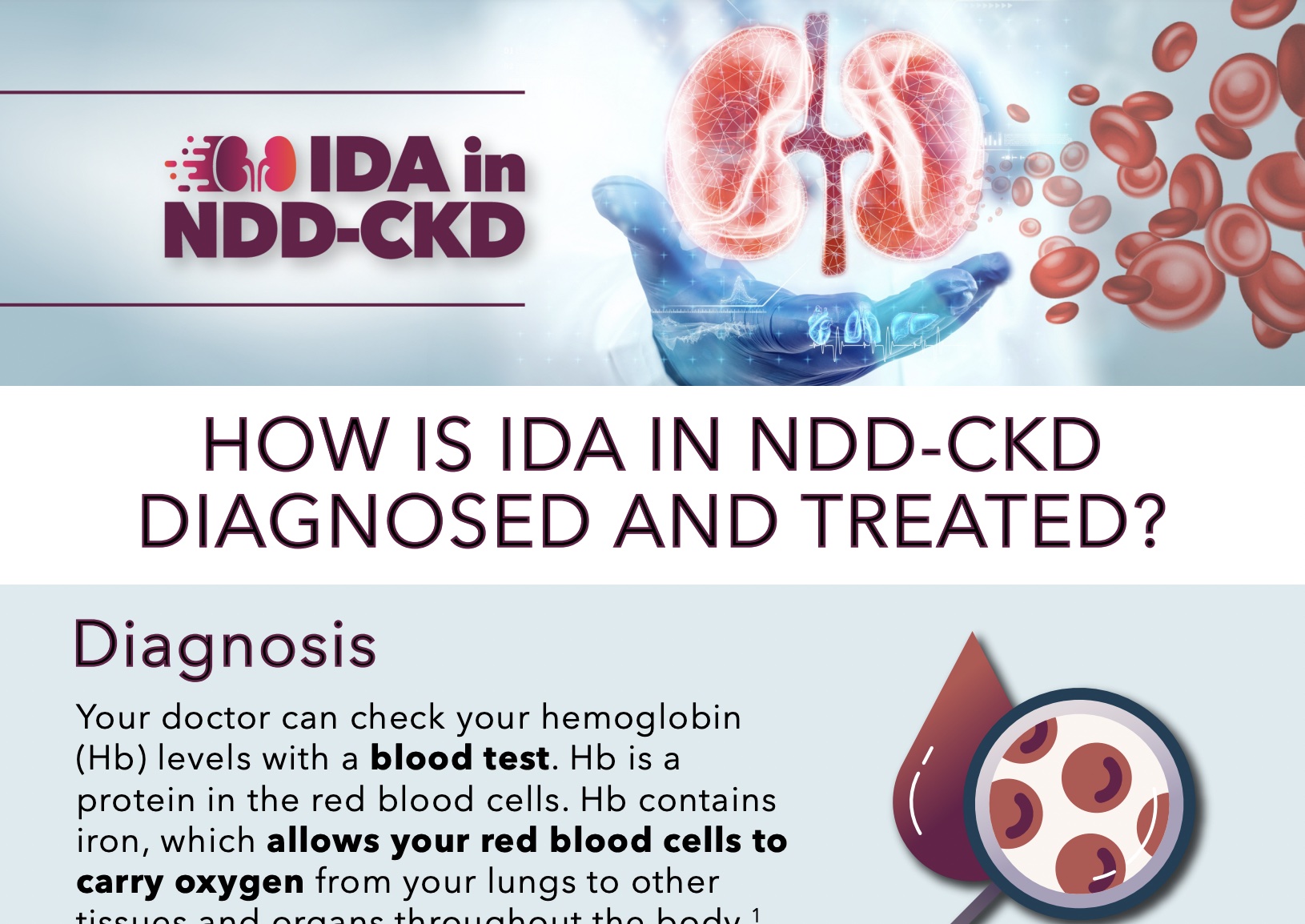
Diagnosis Your doctor can check your hemoglobin (Hb) levels with a blood test. Hb is a protein
Without adequate iron, the body's red blood cells cannot provide enough oxygen to our tissues and organs, resulting in ID. A frequent consequence of CKD is iron-deficiency anemia (IDA). You might have reduced iron levels if you have CKD. Many patients with CKD also experience blood loss that results in iron shortage, particularly if they are receiving dialysis for their renal failure. Due to infections, inflammation, and malnutrition, patients with CKD frequently experience problems with iron absorption.
References:
- Mayo Clinic Website. Iron Deficiency Anemia. Date accessed September 2022. https://www.mayoclinic.org/diseases-conditions/iron-deciency-anemia/symptoms-causes/syc-20355034
- National Institute of Diabetes and Digestive and Kidney Disease Website. Anemia in Chronic Kidney Disease. Date accessed September 2022. https://www.niddk.nih.gov/
Lack of iron in the diet (for example a vegan diet or malnutrition), problems with iron absorption in the stomach, increased blood loss, and an increased need for iron can all contribute to IDA.
References:
- Cappellini MD, Musallam KM, Taher AT. Iron deficiency anaemia revisited. J Intern Med. 2020;287(2):153-170. doi:10.1111/joim.13004
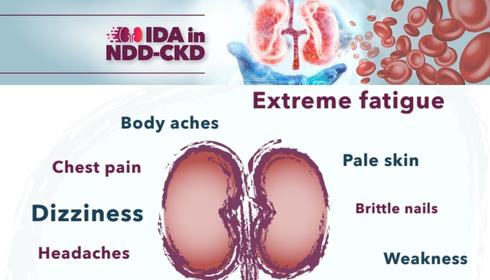
Extreme exhaustion, shortness of breath, pale skin, brittle fingernails, body aches and a weak feeling, headaches, dizziness, fainting, heart palpitations, chest pain, disturbed sleep, and difficulty focusing are possible symptoms of IDA.
References:
- Mayo Clinic Website. Iron Deficiency Anemia. Date accessed September 2022. https://www.mayoclinic.org/diseases-conditions/iron-deciency-anemia/symptoms-causes/syc-20355034
- Fishbane S, Spinowitz B. Update on anemia in ESRD and earlier stages of CKD: Core curriculum 2018. American Journal of Kidney Diseases. 2018;71(3):423–435. doi:10.1053/j.ajkd.2017.09.026
Our bodies need iron to make hemoglobin (Hb). Hb contains iron, which allows it to bind to oxygen. Hb enables your red blood cells to carry oxygen from your lungs to other tissues and organs throughout your body.
References:
- Cleveland Clinic website. Hemoglobin Test. Date updated July 2022. Date accessed August 2022. https://my.clevelandclinic.org/health/diagnostics/17790-hemoglobin-test
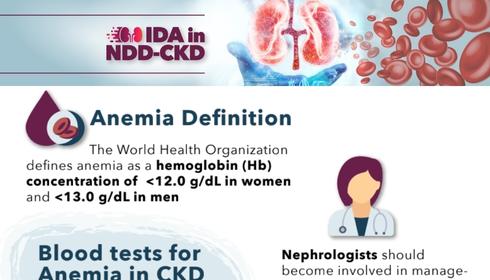
Doctors can suspect IDA from your symptoms. If IDA is suspected, a simple blood test can check the level of Hb in your blood. If your Hb is low, then this indicates that iron levels are low, and IDA can be diagnosed. The World Health Organization defines anemia as a Hb concentration of less than 12.0 g/dL in women and less than 13.0 g/dL in men.
References:
- Cleveland Clinic website. Hemoglobin Test. Date updated July 2022. Date accessed August 2022. https://my.clevelandclinic.org/health/diagnostics/17790-hemoglobin-test
- Fishbane S, Spinowitz B. Update on anemia in ESRD and earlier stages of CKD: Core curriculum 2018. American Journal of Kidney Diseases. 2018;71(3):423–435. doi:10.1053/j.ajkd.2017.09.026
Iron is poorly absorbed from our stomachs and intestines. Most of the iron we take orally is not absorbed into our bodies and can cause side effects. Many people who take iron tablets or capsules get an upset stomach, constipation, or heartburn.
If your iron levels are low and you have kidney disease, iron injections are recommended over iron tablets or capsules because of its fast absorption into your body and less side effects.
References:
- Gafter-Gvili A, Schechter A, Rozen-Zvi B. Iron Deficiency Anemia in Chronic Kidney Disease. Acta Haematol. 2019;142(1):44-50. doi: 10.1159/000496492.
- Pergola PE, Fishbane S, Ganz T. Novel Oral Iron Therapies for Iron Deficiency Anemia in Chronic Kidney Disease. Adv Chronic Kidney Dis. 2019;26(4):272-291. doi:10.1053/j.ackd.2019.05.002
You can increase your iron by eating foods that are rich in iron. It is recommended that you eat an iron-rich diet, which includes foods like meat and leafy green vegetables. There are plenty of other foods that are rich in iron and other foods that contain vitamin C, that help your body to absorb iron more effectively. If your iron levels are slightly low, then your doctor may recommend you increase iron in your diet. If your iron levels are very low and you have IDA, then it may take too long to increase your iron levels through diet alone. An injection with iron can restore your iron levels quickly, reducing the symptoms of IDA more efficiently.
References:
- Healthdirect website. Foods high in iron. Date accessed August 2022. https://www.healthdirect.gov.au/foods-high-in-iron
- Sharecare website. Living well with Anemia. Date updated Sept 2021. Date accessed Aug 2022. https://www.sharecare.com/anemia/habits-maximize-iron-absorption
This initiative is supported by an independent educational grant from American Regent.